维生素 A 棕榈酸酯 | 79-81-2
中文名称
维生素 A 棕榈酸酯
中文别名
视黄醇棕榈酸酯;维生素A棕榈酸酯;维生素A;维A棕榈酸酯
英文名称
retinyl palmitate
英文别名
all-trans-retinol palmitate;vitamin A palmitate;[(2E,4E,6E,8E)-3,7-dimethyl-9-(2,6,6-trimethylcyclohexen-1-yl)nona-2,4,6,8-tetraenyl] hexadecanoate
CAS
79-81-2
化学式
C36H60O2
mdl
——
分子量
524.871
InChiKey
VYGQUTWHTHXGQB-FFHKNEKCSA-N
BEILSTEIN
——
EINECS
——
-
物化性质
-
计算性质
-
ADMET
-
安全信息
-
SDS
-
制备方法与用途
-
上下游信息
-
文献信息
-
表征谱图
-
同类化合物
-
相关功能分类
-
相关结构分类
物化性质
-
熔点:28-29℃
-
沸点:546.51°C (rough estimate)
-
密度:0.9668 (rough estimate)
-
闪点:194℃
-
溶解度:可溶于氯仿(轻微)、乙酸乙酯(轻微)、甲醇(非常轻微)
-
LogP:15.51 at 25℃
-
物理描述:Solid
计算性质
-
辛醇/水分配系数(LogP):13.6
-
重原子数:38
-
可旋转键数:21
-
环数:1.0
-
sp3杂化的碳原子比例:0.69
-
拓扑面积:26.3
-
氢给体数:0
-
氢受体数:2
ADMET
毒理性
◉ 母乳喂养期间使用总结:维生素A(视黄醇)和前维生素A类胡萝卜素是人类母乳的正常成分。哺乳期妇女的推荐膳食摄入量为每天1300微克视黄醇,相比之下,孕期为每天770微克。6个月或以下婴儿的推荐每日摄入量为400微克。维生素A缺乏并不少见,哺乳期间可能需要补充维生素A以达到推荐的每日维生素A摄入量。在发展中国家,孕期和哺乳期补充维生素A并没有降低母乳喂养婴儿的死亡率或贫血风险,但可能与改善抗氧化能力和免疫功能的健康益处有关。哺乳期妇女单次剂量最高可达120,000微克或每日剂量最高可达1500微克,预计不会对母乳喂养的婴儿造成伤害。母亲应避免每日剂量超过3000微克。
母乳中的维生素A具有抗氧化性质。Holder巴氏杀菌法(62.5°C,30分钟)不会降低牛奶的抗氧化能力。
◉ 对母乳喂养婴儿的影响:印度100名纯母乳喂养的母亲在分娩后24小时内单次口服200,000 IU维生素A或安慰剂。两组婴儿在产后住院期间的体重增长没有差异,维生素A组的婴儿没有出现维生素A过量的症状,如过度哭泣、囟门隆起和呕吐。所有婴儿在出生后48至72小时接受了口服脊髓灰质炎疫苗(OPV)。两组在6周时的OPV血清转化率或抗体滴度没有差异。同样,加纳1,085名纯母乳喂养的母亲在产后3至4周接受了200,000 IU维生素A或安慰剂。在6周和6个月大时,婴儿对脊髓灰质炎或破伤风疫苗接种的免疫反应没有差异。
冈比亚197名母亲在分娩后第一周给予200,000或400,000 IU维生素A,12个月的随访期间未出现维生素A不良反应的迹象。
中国南京245名健康、纯母乳喂养的母亲在产后1至2个月随机接受每日1800 IU维生素A补充剂或安慰剂,持续2个月。在2个月研究结束时,两组婴儿的发热性疾病、呼吸道感染、腹泻和湿疹的发生率相似,尽管没有说明这些数据是如何收集的。
◉ 对泌乳和母乳的影响:坦桑尼亚的HIV感染母亲在孕期和产后服用每日维生素A补充剂时,严重亚临床乳腺炎的发病率(36%)高于服用安慰剂的母亲(23%)。服用不含维生素A的多种维生素的母亲也有较高的发病率(38%),这表明与维生素A无关的影响。鉴于多种维生素补充剂对这一特定病人群体有许多其他益处,作者不建议因乳腺炎的风险而避免补充。
在一项巴西研究中,57名母亲在分娩后2天内接受了200,000 IU维生素A或未接受维生素A。在给药后24小时,接受维生素A的母亲初乳中的平均α-生育酚(维生素E)水平降低了16.4%(28微摩尔/升与24.5微摩尔/升),但在给药后30天,大约6微摩尔/升时,差异不再显著。该研究中报告的维生素E初乳水平在正常范围内,因此维生素A补充剂母亲的轻微降低可能不具有临床意义。一个不同的巴西研究小组使用添加了低剂量维生素E 110 IU作为防腐剂的维生素A补充剂进行了相同的实验,发现维生素A对初乳α-生育酚没有影响。
◉ Summary of Use during Lactation:Vitamin A (retinol) and provitamin A carotenoids are normal components of human milk. The recommend dietary intake in lactating women is 1300 mcg retinol daily, compared to 770 mcg daily during pregnancy. The recommended daily intake for infants aged 6 months or less is 400 mcg. Vitamin A deficiency is not uncommon, and maternal supplementation may be needed during lactation to achieve the recommended daily vitamin A intake. Maternal vitamin A supplementation during pregnancy and lactation has not reduced mortality or the risk of anemia in breastfed infants living in developing regions, but there may be health benefits related to improved antioxidant capacity and immune function. Maternal single doses up to 120,000 mcg or daily doses up to 1500 mcg are not expected to harm the breastfed infant. Daily doses above 3,000 mcg should be avoided in the mother.
Vitamin A in milk has antioxidant properties. Holder pasteurization (62.5 degrees C for 30 minutes) does not reduce milk antioxidant capacity.
◉ Effects in Breastfed Infants:One hundred exclusively breastfeeding mothers in India were given 200,000 IU vitamin A or placebo as a single oral dose within 24 hours after delivery. There were no differences in weight gain of their infants during postpartum hospitalization between the groups, and no infants in the vitamin A group had symptoms of hypervitaminosis A, such as excessive crying, raised fontanelle and vomiting. All the infants received a dose of oral polio vaccine (OPV) between 48 and 72 hours after birth. There were no differences between the two groups in OPV seroconversion rates or antibody titers at 6 weeks. Similarly, 1,085 exclusively breastfeeding mothers in Ghana were given 200,000 IU vitamin A or placebo at 3 to 4 weeks postpartum. There were no differences in infant immune response to polio or tetanus vaccination at 6 weeks and 6 months of age.
The infants of 197 mothers in Gambia given either 200,000 or 400,000 IU vitamin A in the first week after delivery showed no signs of adverse reactions to vitamin A during the 12-month follow-up period.
Two hundred forty-five healthy, exclusively breastfeeding mothers in Nanjing, China were randomized to receive a daily vitamin A 1800 IU supplement or placebo for 2 months beginning at 1 to 2 months postpartum. By the end of the 2 month study, infants in both groups had similar rates of febrile illnesses, respiratory tract infections, diarrhea, and eczema, although it was not stated how these data were collected.
◉ Effects on Lactation and Breastmilk:HIV-infected mothers in Tanzania had a higher rate of severe subclinical mastitis (36%), determined by measuring serial milk electrolyte concentrations, when taking a daily vitamin A supplement during pregnancy and postpartum compared to placebo (23%). Mothers taking a multivitamin without vitamin A also had a higher rate (38%) than placebo, suggesting a vitamin A-independent effect. Given the many other benefits of multivitamin supplementation in this specific patient population, the authors did not recommend avoiding supplementation due to a potential risk of mastitis.
In a Brazilian study, 57 mothers received either 200,000 IU vitamin A or no vitamin A within 2 days after birth. At 24 hours after administration, the average level of alpha-tocopherol (vitamin E) was 16.4% lower in the colostrum of mothers who received in the vitamin A (28 micromoles/L compared to 24.5 micromoles/L), but it was not significantly different at 30 days after administration, at about 6 micromoles/L. The reported vitamin E colostrum levels in this study are within normal limits, thus the small reduction in the vitamin A-supplemented mothers may not be clinically important. A different Brazilian research group conducting the same experiment using a vitamin A supplement with low-dose vitamin E 110 IU added as a preservative found no effect of vitamin A on colostrum alpha-tocopherol.
来源:Drugs and Lactation Database (LactMed)
安全信息
-
TSCA:Yes
-
危险品标志:Xn
-
安全说明:S23,S36/37,S36/37/39,S45,S53
-
危险类别码:R63
-
WGK Germany:3
-
海关编码:2936210000
-
危险品运输编号:UN1170 - class 3 - PG 2 - Ethanol, solution
-
RTECS号:VH6860000
-
储存条件:本品应充氮气密封并在4℃下保存。
SDS
模块 1. 化学品
1.1 产品标识符
: Retinyl palmitate
产品名称
1.2 鉴别的其他方法
Vitamin A palmitate
all−trans−Retinol palmitate
1.3 有关的确定了的物质或混合物的用途和建议不适合的用途
仅用于研发。不作为药品、家庭或其它用途。
模块 2. 危险性概述
2.1 GHS-分类
生殖毒性 (类别 1B)
慢性水生毒性 (类别 4)
2.2 GHS 标记要素,包括预防性的陈述
象形图
警示词 危险
危险申明
H360 可能对生育能力或胎儿造成伤害。
H413 可能对水生生物产生长期持续的有害影响。
警告申明
预防措施
P201 在使用前获取特别指示。
P202 在读懂所有安全防范措施之前切勿操作。
P273 避免释放到环境中。
P280 戴防护手套/穿防护服/戴护目镜/戴面罩.
事故响应
P308 + P313 如接触到或有疑虑:求医/ 就诊。
安全储存
P405 存放处须加锁。
废弃处置
P501 将内容物/ 容器处理到得到批准的废物处理厂。
只限于专业使用者。
2.3 其它危害物 - 无
模块 3. 成分/组成信息
3.1 物 质
: Vitamin A palmitate
别名
all−trans−Retinol palmitate
: C36H60O2
分子式
: 524.86 g/mol
分子量
组分 浓度或浓度范围
Retinyl palmitate
<=100%
化学文摘登记号(CAS 79-81-2
No.) 201-228-5
EC-编号
模块 4. 急救措施
4.1 必要的急救措施描述
一般的建议
请教医生。 向到现场的医生出示此安全技术说明书。
吸入
如果吸入,请将患者移到新鲜空气处。 如呼吸停止,进行人工呼吸。 请教医生。
皮肤接触
用肥皂和大量的水冲洗。 请教医生。
眼睛接触
用水冲洗眼睛作为预防措施。
食入
切勿给失去知觉者通过口喂任何东西。 用水漱口。 请教医生。
4.2 主要症状和影响,急性和迟发效应
过度接触产生的急性症状包括:, 烦躁, 呕吐, 食欲减退, 头痛, 红斑
4.3 及时的医疗处理和所需的特殊处理的说明和指示
无数据资料
模块 5. 消防措施
5.1 灭火介质
灭火方法及灭火剂
用水雾,抗乙醇泡沫,干粉或二氧化碳灭火。
5.2 源于此物质或混合物的特别的危害
碳氧化物
5.3 给消防员的建议
如必要的话,戴自给式呼吸器去救火。
5.4 进一步信息
无数据资料
模块 6. 泄露应急处理
6.1 作业人员防护措施、防护装备和应急处置程序
使用个人防护用品。 避免吸入蒸气、烟雾或气体。 保证充分的通风。 人员疏散到安全区域。
6.2 环境保护措施
如能确保安全,可采取措施防止进一步的泄漏或溢出。 不要让产品进入下水道。
一定要避免排放到周围环境中。
6.3 泄漏化学品的收容、清除方法及所使用的处置材料
用惰性吸附材料吸收并当作危险废物处理。 放入合适的封闭的容器中待处理。
6.4 参考其他部分
丢弃处理请参阅第13节。
模块 7. 操作处置与储存
7.1 安全操作的注意事项
避免曝露:使用前需要获得专门的指导。避免吸入蒸气和烟雾。
7.2 安全储存的条件,包括任何不兼容性
贮存在阴凉处。 使容器保持密闭,储存在干燥通风处。
打开了的容器必须仔细重新封口并保持竖放位置以防止泄漏。
建议的贮存温度: 2 - 8 °C
充气保存 对光和空气敏感
7.3 特定用途
无数据资料
模块 8. 接触控制和个体防护
8.1 容许浓度
最高容许浓度
没有已知的国家规定的暴露极限。
8.2 暴露控制
适当的技术控制
根据良好的工业卫生和安全规范进行操作。 休息前和工作结束时洗手。
个体防护设备
眼/面保护
带有防护边罩的安全眼镜符合 EN166要求请使用经官方标准如NIOSH (美国) 或 EN 166(欧盟)
检测与批准的设备防护眼部。
皮肤保护
戴手套取 手套在使用前必须受检查。
请使用合适的方法脱除手套(不要接触手套外部表面),避免任何皮肤部位接触此产品.
使用后请将被污染过的手套根据相关法律法规和有效的实验室规章程序谨慎处理. 请清洗并吹干双手
所选择的保护手套必须符合EU的89/686/EEC规定和从它衍生出来的EN 376标准。
完全接触
物料: 丁腈橡胶
最小的层厚度 0.11 mm
溶剂渗透时间: 480 min
测试过的物质Dermatril® (KCL 740 / Z677272, 规格 M)
飞溅保护
物料: 丁腈橡胶
最小的层厚度 0.11 mm
溶剂渗透时间: 480 min
测试过的物质Dermatril® (KCL 740 / Z677272, 规格 M)
, 测试方法 EN374
如果以溶剂形式应用或与其它物质混合应用,或在不同于EN
374规定的条件下应用,请与EC批准的手套的供应商联系。
这个推荐只是建议性的,并且务必让熟悉我们客户计划使用的特定情况的工业卫生学专家评估确认才可.
这不应该解释为在提供对任何特定使用情况方法的批准.
身体保护
防渗透的衣服, 防护设备的类型必须根据特定工作场所中的危险物的浓度和数量来选择。
呼吸系统防护
如危险性评测显示需要使用空气净化的防毒面具,请使用全面罩式多功能防毒面具(US)或ABEK型
(EN
14387)防毒面具筒作为工程控制的候补。如果防毒面具是保护的唯一方式,则使用全面罩式送风防
毒面具。 呼吸器使用经过测试并通过政府标准如NIOSH(US)或CEN(EU)的呼吸器和零件。
模块 9. 理化特性
9.1 基本的理化特性的信息
a) 外观与性状
形状: 粘性的
b) 气味
无数据资料
c) 气味阈值
无数据资料
d) pH值
无数据资料
e) 熔点/凝固点
熔点/凝固点: 大约26 °C
f) 沸点、初沸点和沸程
大约100 °C
g) 闪点
194 °C - 闭杯
h) 蒸发速率
无数据资料
i) 易燃性(固体,气体)
无数据资料
j) 高的/低的燃烧性或爆炸性限度 无数据资料
k) 蒸气压
无数据资料
l) 蒸汽密度
无数据资料
m) 密度/相对密度
921.1 kg/m3 在 20 °C
n) 水溶性
0.001 g/l 在 25 °C
o) n-辛醇/水分配系数
辛醇--水的分配系数的对数值: 10.3
p) 自燃温度
261 °C 在 1,006 - 1,014 hPa
q) 分解温度
无数据资料
r) 粘度
无数据资料
模块 10. 稳定性和反应活性
10.1 反应性
无数据资料
10.2 稳定性
无数据资料
10.3 危险反应
无数据资料
10.4 应避免的条件
无数据资料
10.5 不相容的物质
无数据资料
10.6 危险的分解产物
其它分解产物 - 无数据资料
模块 11. 毒理学资料
11.1 毒理学影响的信息
急性毒性
半数致死剂量 (LD50) 经口 - 大鼠 - 雄性和雌性 - > 2,000 mg/kg
皮肤刺激或腐蚀
皮肤 - 兔子 - 无皮肤刺激 - 4 h - 经济合作与发展组织的试验指南404
眼睛刺激或腐蚀
眼睛 - 兔子 - 无眼睛刺激 - 72 h - 经济合作与发展组织的试验指南405
呼吸道或皮肤过敏
过敏原的最大化试验 - 豚鼠 - 不引起皮肤过敏。 - 经济合作与发展组织的试验指南406
生殖细胞致突变性
细胞突变性-体外试验 - Ames 试验(艾姆斯试验) - 鼠伤寒沙门氏菌 - 有或没有代谢活化作用 - 阴性
细胞突变性-体内试验 - 小鼠 - 雄性 - 经口 - 阴性
致癌性
IARC:
此产品中没有大于或等于 0。1%含量的组分被 IARC鉴别为可能的或肯定的人类致癌物。
生殖毒性
有可能会损害胎儿。 假设的人类生殖毒物
发育毒性 - 猴子 - 经口
特定发育异常:眼、耳。 特定发育异常:其他发育异常。
发育毒性 - 大鼠 - 经口
特定发育异常:眼、耳。 特定发育异常:颅面(包括鼻和舌)。 特定发育异常:肌肉骨骼系统。
特异性靶器官系统毒性(一次接触)
无数据资料
特异性靶器官系统毒性(反复接触)
无数据资料
吸入危险
无数据资料
潜在的健康影响
吸入 吸入可能有害。 可能引起呼吸道刺激。
摄入 如服入是有害的。
皮肤 通过皮肤吸收可能有害。 可能引起皮肤刺激。
眼睛 可能引起眼睛刺激。
接触后的征兆和症状
过度接触产生的急性症状包括:, 烦躁, 呕吐, 食欲减退, 头痛, 红斑
附加说明
反复染毒毒性 - 大鼠 - 雄性 - 经口 - 未观察到有害效果的水平 - 1.43 - 3.32 mg/kg - 观察到有害效果的最低水平
- 5.77 - 12.97 mg/kg
化学物质毒性作用登记: 无数据资料
模块 12. 生态学资料
12.1 生态毒性
对鱼类的毒性 静态试验 半数致死浓度(LC50) - 高体雅罗鱼 (金雅罗鱼) - > 10,000 mg/l -
96 h
方法: 德国工业标准(DIN)38412
对水蚤和其他水生无脊 静态试验 半数效应浓度(EC50) - 大型蚤 (水蚤) - > 100 mg/l - 48 h
椎动物的毒性 方法: 经济合作和发展组织的试验指导书202
对藻类的毒性 静态试验 半数效应浓度(EC50) - 近具刺链带藻 (绿藻) - 152.94 mg/l - 72 h
12.2 持久性和降解性
生物降解能力 好氧的 - 接触时间 28 d
结果: 50 - 60 % - 可部分生物降解
12.3 潜在的生物累积性
无数据资料
12.4 土壤中的迁移性
无数据资料
12.5 PBT 和 vPvB的结果评价
无数据资料
12.6 其它不良影响
模块 13. 废弃处置
13.1 废物处理方法
产品
将剩余的和不可回收的溶液交给有许可证的公司处理。
受污染的容器和包装
按未用产品处置。
模块 14. 运输信息
14.1 联合国危险货物编号
欧洲陆运危规: - 国际海运危规: - 国际空运危规: -
14.2 联合国运输名称
欧洲陆运危规: 非危险货物
国际海运危规: 非危险货物
国际空运危规: 非危险货物
14.3 运输危险类别
欧洲陆运危规: - 国际海运危规: - 国际空运危规: -
14.4 包裹组
欧洲陆运危规: - 国际海运危规: - 国际空运危规: -
14.5 环境危险
欧洲陆运危规: 否 国际海运危规 国际空运危规: 否
海洋污染物(是/否): 否
14.6 对使用者的特别提醒
无数据资料
模块 15 - 法规信息
N/A
模块16 - 其他信息
N/A
制备方法与用途
简介
视黄醇棕榈酸酯(Retinyl palmitate)是一种维生素A的衍生物,它是视黄醇(retinol)与棕榈酸(palmitic acid)结合形成的酯。棕榈酸是饱和脂肪酸,主要存在于棕榈油中。视黄醇棕榈酸酯易于被皮肤吸收并转化为视黄醇,是一种黄色或黄红色的固体或油状物质。
应用维生素A棕榈酸酯眼用凝胶(兹养)在临床上应用广泛。它主要用于修复杯状细胞功能,并逆转细胞角化。结膜杯状细胞是结膜上皮层的重要组成部分,主要负责分泌黏蛋白以保护和润滑眼表。过敏性结膜炎、干燥综合征及烧伤等引起的结膜炎症会损伤杯状细胞,进而导致黏蛋白层异常。
生物活性Retinyl (维生素A) Palmitate是一种更为稳定的维生素A衍生物,将必需营养素维生素A与棕榈酸结合。
体外研究由明胶-阿拉伯树胶复合材料微囊化制成的视黄醇棕榈酸酯具有潜在的优势。这种方法能够将油性的维生素A转化为固体粉末,便于处理和制备混合物。
体内研究在小鼠乳突淋瘤模型中,维生素A棕榈酸酯以每天80 mg/kg或每周一次800 mg/kg的剂量口服给药时,显示出剂量依赖性地缩小肿瘤的效果。与单纯口服维生素A酸相比,在相同总剂量下,每日给药比每周给药能产生更显著的退化效果。此外,一次性注射150克维生素A棕榈酸酯在预先免疫接种绵羊红细胞(SRBC)后增强了细胞介导的免疫力,并且这种增强作用至少持续3周。
用途视黄醇棕榈酸酯能透皮吸收,抗角质化,刺激胶原蛋白和弹性蛋白的增长,增加表皮及真皮的厚度。它还能够提升皮肤弹性、减少皱纹、促进皮肤更新并保持皮肤活力,适用于眼霜、保湿霜、修护霜、洗发水以及护发素等产品中。
上下游信息
-
上游原料
中文名称 英文名称 CAS号 化学式 分子量 维生素 A 醋酸酯 Retinol acetate 127-47-9 C22H32O2 328.495 —— 3-methyl-5-acetoxy-1-(2,6,6-trimethyl-1-cyclohexen-1-yl)-1,3-pentadiene 3917-38-2 C17H26O2 262.392 维生素A RETINOL 68-26-8 C20H30O 286.458 (2E,4Z,6E,8E)-3,7-二甲基-9-(2,6,6-三甲基-1-环己烯基)壬-2,4,6,8-四烯-1-醇 11-cis-retinol 22737-96-8 C20H30O 286.458 (7E,9E)-beta-离子亚基乙醛 (2E,4E)-3-methyl-5-(2,6,6-trimethyl-1-cyclohexen-1-yl)-2,4-pentadienal 3917-41-7 C15H22O 218.339 —— 3-methyl-5-chloro-1-(2,6,6-trimethyl-1-cyclohexen-1-yl)-1,3-pentadiene 55732-70-2 C15H23Cl 238.801 —— 3-methyl-5-bromo-1-(2,6,6-trimethyl-1-cyclohexen-1-yl)-1,3-pentadiene 38987-92-7 C15H23Br 283.252 -
下游产品
中文名称 英文名称 CAS号 化学式 分子量 —— retinol —— C20H30O 286.458 维生素A RETINOL 68-26-8 C20H30O 286.458 —— 3,7-dimethyl-9-(2,6,6-trimethyl-1-cyclohexen-1-yl)-2,4,6,8-nontetraen-1-ol 34218-73-0 C20H30O 286.458 (2E,4Z,6E,8E)-3,7-二甲基-9-(2,6,6-三甲基-1-环己烯基)壬-2,4,6,8-四烯-1-醇 11-cis-retinol 22737-96-8 C20H30O 286.458 异维A酸 13-cis-retinoic acid 4759-48-2 C20H28O2 300.441 维A酸 all-trans-retinoic-acid 302-79-4 C20H28O2 300.441 —— 20,14-retro-Retinoic acid 138093-35-3 C20H28O2 300.441 —— 14-Ethylretinoic acid 138093-41-1 C22H32O2 328.495 —— 13-cis-14-Isopropylretinoic acid 138231-99-9 C23H34O2 342.522 —— 14-Isopropylretinoic acid 138093-42-2 C23H34O2 342.522
反应信息
-
作为反应物:描述:参考文献:名称:视黄酸的碱催化异构化。14-烷基化的全反式,13-顺式和20,14-复古-视黄酸的合成和诱导分化的活性。摘要:视黄酸(1)通过过量的二异丙基氨基锂(LDA)进行区域选择性异构化,得到20,14-复古视黄酸(3)。视黄酸的中间二价阴离子的烷基化得到3的14-烷基化衍生物。通过在碱性条件下烷基化的逆向异构体的异构化,合成了几种14-烷基-全反式和-13-顺式-视黄酸。基于诱导人早幼粒细胞白血病细胞系HL-60分化的能力,检查了这些衍生物的类维生素A活性。20,14-复古视黄酸(3)的活性是视黄酸(1)的1/50。虽然14-甲基-20,14-复古-视黄酸(4)具有3的活性,但将14-甲基引入全反式和13-顺式-视黄酸会降低活性。DOI:10.1021/jm00081a020
-
作为产物:描述:β-cyclogeranyl chloride 在 sodium methylate 、 sodium ethanolate 、 sodium hydroxide 作用下, 以 二氯甲烷 、 水 、 N,N-二甲基甲酰胺 、 乙腈 为溶剂, 反应 19.0h, 生成 维生素 A 棕榈酸酯参考文献:名称:一种维生素A酯中间体C15及维生素A酯的制备方法摘要:本发明提供一种维生素A酯中间体C15及维生素A酯的制备方法。该方法以3,7‑二甲基‑3‑羟基‑1,6‑辛二烯为起始原料,经卤代反应、环化反应,然后和三苯基膦或亚磷酸三酯经取代反应制备相应Wittig试剂,然后和2‑甲基‑4‑乙酰氧基‑2‑丁烯醛经Wittig反应、酸化,所得产物经水解和酸化,再和三苯基膦或亚磷酸三酯经取代反应制备C15。利用所得C15和2‑甲基‑4‑R3取代基羰基氧基‑2‑丁烯醛经Wittig反应可制备维生素A酯。本发明方法反应类型单一,反应条件易于操作和实现,操作安全环保,后处理简单,成本较低;反应活性强,反应选择性高,原子经济性高,目标产物收率和纯度高。公开号:CN111484525B
文献信息
-
[EN] NOVEL THYROMIMETICS<br/>[FR] NOUVEAUX THYROMIMÉTIQUES申请人:AUTOBAHN THERAPEUTICS INC公开号:WO2021108549A1公开(公告)日:2021-06-03Compounds are provided having the structure of Formula (I) or a pharmaceutically acceptable isomer, racemate, hydrate, solvate, isotope, or salt thereof, wherein R1, R2, X1, X2, Y1, and Y2 are as defined herein. Such compounds function as thyromimetics and have utility for treating diseases such as neurodegenerative disorders and fibrotic diseases. Pharmaceutical compositions containing such compounds are also provided, as are methods of their use and preparation.提供具有Formula (I)结构或其药学上可接受的异构体、拉克酸盐、水合物、溶剂化合物、同位素或盐的化合物,其中R1、R2、X1、X2、Y1和Y2如本文所定义。这些化合物作为甲状腺类似物发挥作用,并可用于治疗神经退行性疾病和纤维化疾病等疾病。还提供含有这些化合物的药物组合物,以及它们的使用和制备方法。
-
[EN] DERIVATIVES OF AMANITA TOXINS AND THEIR CONJUGATION TO A CELL BINDING MOLECULE<br/>[FR] DÉRIVÉS DE TOXINES D'AMANITES ET LEUR CONJUGAISON À UNE MOLÉCULE DE LIAISON CELLULAIRE申请人:HANGZHOU DAC BIOTECH CO LTD公开号:WO2017046658A1公开(公告)日:2017-03-23Derivatives of Amernita toxins of Formula (I), wherein, formula (a) R 1, R 2, R 3, R 4, R 5, R 6, R 7, R 8, R 9, R 10, X, L, m, n and Q are defined herein. The preparation of the derivatives. The therapeutic use of the derivatives in the targeted treatment of cancers, autoimmune disorders, and infectious diseases.
-
POLYETHYLENE GLYCOL DERIVATIVES OF PALMITOYLETHANOLAMIDE AND ANALOGOUS ACYLETHANOLAMIDES申请人:EPITECH GROUP S.r.l.公开号:US20150157733A1公开(公告)日:2015-06-11The synthesis of a series of Polyethylene glycol conjugates (esters and carbonates) of PEA and its analogous acylethanolamides, have higher water solubility and good hydrophilic/lipophilic balance, resulting in (i) improved accumulation in tissues (particularly skin and mucosae), (ii) prolonged release, and (iii) increased bioavailability. Improvement of PEA and analogous acylethanolamides levels in the tissues—particularly in the skin and mucosae—and their prolonged release is due to the improved bioavailability of related conjugates. Conjugates are able to extend the time frame in which PEA and analogous acylethanolamides exert their pharmacological effects.
-
COMPOUNDS AND USES THEREOF申请人:Yumanity Therapeutics, Inc.公开号:US20190330198A1公开(公告)日:2019-10-31The present invention features compounds useful in the treatment of neurological disorders. The compounds of the invention, alone or in combination with other pharmaceutically active agents, can be used for treating or preventing neurological disorders.本发明涉及用于治疗神经系统疾病的化合物。本发明的化合物可以单独或与其他药用活性剂结合使用,用于治疗或预防神经系统疾病。
-
[EN] COMPOSITIONS AND METHODS FOR THE TREATMENT OF BACTERIAL INFECTIONS<br/>[FR] COMPOSÉS ET MÉTHODES POUR LE TRAITEMENT D'INFECTIONS BACTÉRIENNES申请人:CIDARA THERAPEUTICS INC公开号:WO2018006063A1公开(公告)日:2018-01-04Compositions and methods for the treatment of bacterial infections include compounds containing dimers of cyclic heptapeptides conjugated to one or more monosaccharide or oligosaccharide moieties. In particular, compounds can be used in the treatment of bacterial infections caused by Gram-negative bacteria.
表征谱图
-
氢谱1HNMR
-
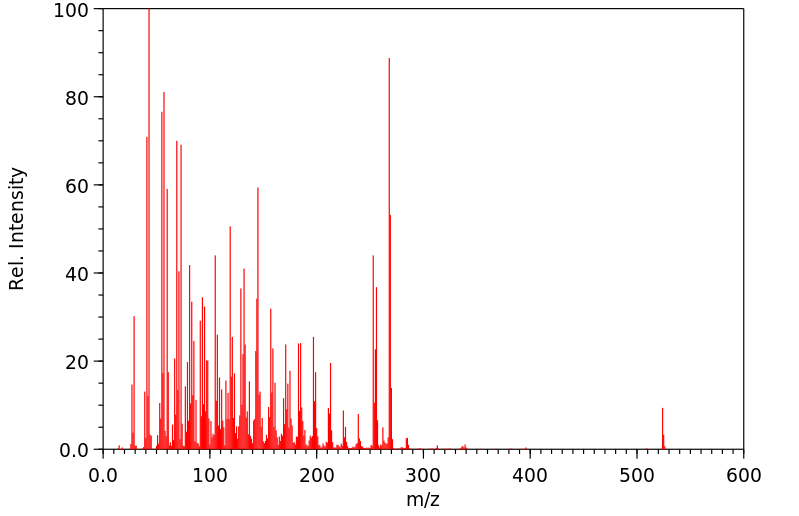
质谱MS
-
碳谱13CNMR
-
红外IR
-
拉曼Raman
-
峰位数据
-
峰位匹配
-
表征信息
同类化合物
(±)17,18-二HETE
(±)-辛酰肉碱氯化物
(Z)-5-辛烯甲酯
(Z)-4-辛烯酸
(R)-甲羟戊酸锂盐
(R)-普鲁前列素,游离酸
(R,R)-半乳糖苷
(E)-4-庚烯酸
(E)-4-壬烯酸
(E)-4-十一烯酸
(9Z,12E)-十八烷二烯酸甲酯
(6E)-8-甲基--6-壬烯酸甲基酯-d3
(3R,6S)-rel-8-[2-(3-呋喃基)-1,3-二氧戊环-2-基]-3-羟基-2,6-二甲基-4-辛酮
龙胆二糖
黑曲霉二糖
黄质霉素
麦芽酮糖一水合物
麦芽糖醇
麦芽糖酸
麦芽糖基蔗糖
麦芽糖一水合物
麦芽糖
鳄梨油酸乙酯
鲸蜡醇蓖麻油酸酯
鲸蜡醇油酸酯
鲸蜡硬脂醇硬脂酸酯
鲸蜡烯酸脂
鲸蜡基花生醇
鲫鱼酸
鲁比前列素
鲁比前列素
高级烷基C16-18-醇
高甲羟戊酸
高效氯氰菊酯
高-gamma-亚油酸
马来酸烯丙酯
马来酸氢异丙酯
马来酸氢异丁酯
马来酸氢丙酯
马来酸氢1-[2-(2-羟基乙氧基)乙基]酯
马来酸单乙酯
马来酸单丁酯
马来酸二辛酯
马来酸二癸酯
马来酸二甲酯
马来酸二烯丙酯
马来酸二正丙酯
马来酸二戊基酯
马来酸二异壬酯
马来酸二异丙酯