代谢
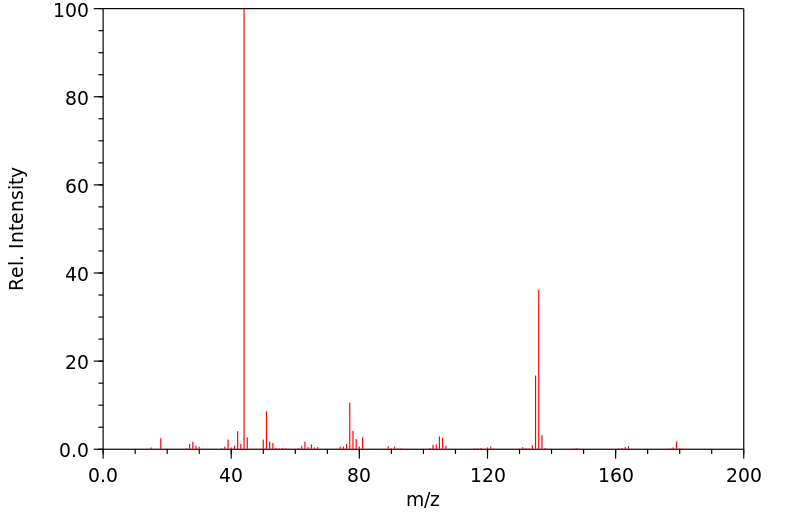
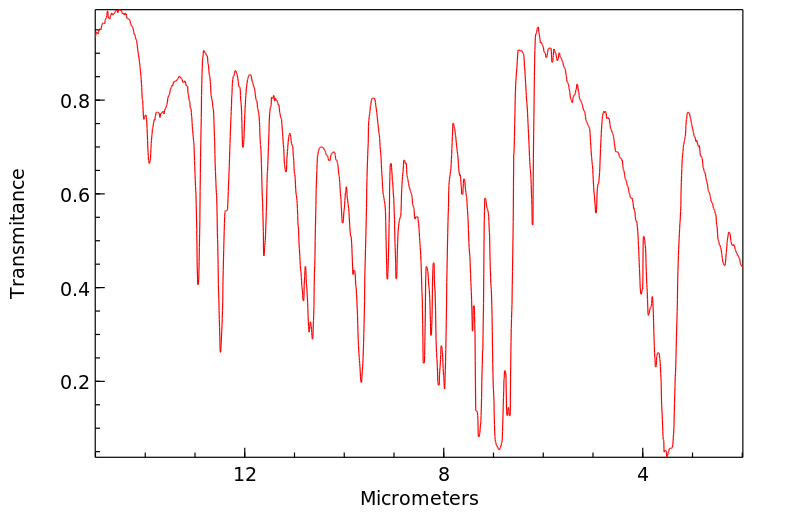
设计药物甲氧基安非他明(MDA)、R,S-甲氧基甲基安非他明(MDMA)、R,S-甲氧基乙基安非他明(MDE)、R, S-苯并二氧杂唑基丁胺(BDB)和R, S-N-甲基-苯并二氧杂唑基丁胺(MBDB)的一相和二相代谢物通过气相色谱-质谱(GC-MS)或液相色谱-质谱(LC-MS)在人类和大鼠的尿液和肝脏微粒体中进行了鉴定。可以假设出两个重叠的途径:(1)去甲基化随后通过儿茶酚-O-甲基转移酶(COMT)催化的甲基化以及/或葡萄糖醛酸化/硫酸化;(2)N-脱烷基化、脱氨,仅对于MDA、MDMA、MDE,氧化为相应的苯甲酸衍生物与甘氨酸结合。去甲基化主要由CYP2D1/6或CYP3A2/4催化,但也可以通过CYP独立机制进行。在人类中,MDMA和MBDB也可以通过CYP1A2去甲基化。N-脱甲基化主要由CYP1A2催化,N-脱乙基化由CYP3A2/4催化。...
The phase I and II metabolites of the designer drugs methylenedioxyamphetamine (MDA), R,S-methylenedioxymethamphetamine (MDMA), R,S-methylenedioxyethylamphetamine (MDE), R, S-benzodioxazolylbutanamine (BDB) and R, S-N-methyl-benzodioxazolylbutanamine (MBDB) were identified by gas chromatography-mass spectrometry (GC-MS) or liquid chromotography-mass spectrometry (LC-MS) in urine and liver microsomes of humans and rats. Two overlapping pathways could be postulated: (1) demethylenation followed by catechol-O-methyl-transferase (COMT) catalyzed methylation and/or glucuronidation/sulfatation; (2) N-dealkylation, deamination and only for MDA, MDMA, MDE oxidation to the corresponding benzoic acid derivatives conjugated with glycine. Demethylenation was mainly catalyzed by CYP2D1/6 or CYP3A2/4, but also by CYP independent mechanisms. In humans, MDMA and MBDB could also be demethylenated by CYP1A2. N-demethylation was mainly catalyzed by CYP1A2, N-deethylation by CYP3A2/4. ...
来源:Hazardous Substances Data Bank (HSDB)